Normal respiration rate is about 12 breaths per minute (bpm), yet most people breathe at 18 bpm. Fast breathing is known to stimulate the sympathetic nervous system which over time can strain the cardiovascular system. Respiration rate, much like heart rate, is a marker for pulmonary dysfunction.
Using mindfulness principles, Cardiowell increases a person's wellness by helping them breathe slower. Over time with increased awareness and better breathing, people's wellbeing increases and their blood pressure becomes more stable.
Cardiowell Solution
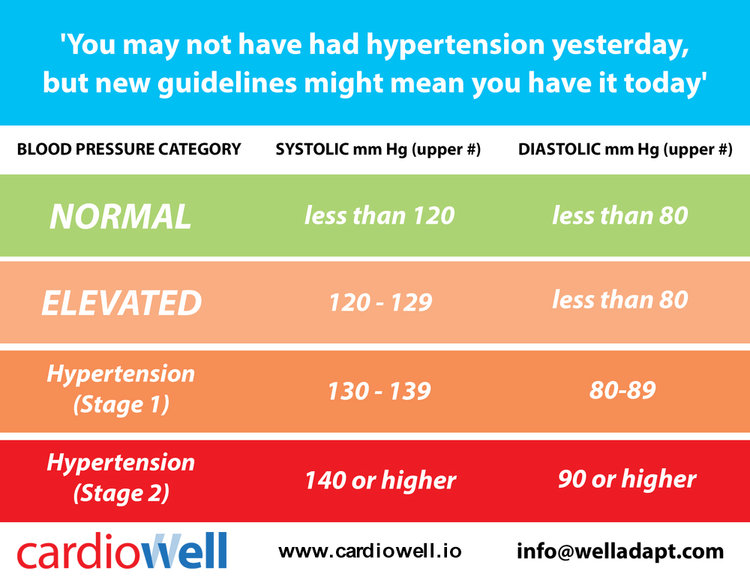
Cardiowell combines remote monitoring and medication management with wellness and mindfulness to lower blood pressure. Cardiowell expects to help lower blood pressure from at least 140/90 mmHg to the newly recommended 120/80 mmHg. Based on research, this is projected to help reduce the rate of stroke by around 25% and heart attacks by 20%.5
The greatest predictor of a second heart attack or stroke is having uncontrolled blood pressure. Cardiowell can also be used by patient-centered homes allowing chronic disease patients and post-acute patients to be remotely cared for. Patients benefit from having to take fewer medications thus decreasing the number of side effects, while at the same time it helps payers reduce population risks and costs.
Cardiowell is available today for employers and consumers as part of a physician-led care plan to help reduce the risks associated with hypertension. Learn more at www.cardiowell.io
Download the PDF version of the article here:
Hypertension is the Biggest Cost Center Being Faced by Healthcare Today (2017)
Reducing blood pressure is the key to managing the exploding chronic disease crisis in the United States.
References:
1. Kung, H. C., & Xu, J. (2015). Hypertension-related Mortality in the United States, 2000-2013. NCHS data brief, (193), 1-8. View article
2. Chockalingam, A., Campbell, N. R., & Fodor, J. G. (2006). Worldwide Epidemic of Hypertension. Canadian Journal of Cardiology, 22(7), 553-555. View article
3. Milliman Client Report(2005). The Need for Better Hypertension Control: Addressing Gaps in Care with the Medical Home Model. Milliman, Inc., NY. View article
4. Comstock, J. (2015). Intel's Medical Director: Hypertension is Mobile Health's Biggest Opportunity. View article
5. SPRINT Research Group. (2015). A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med, 2015(373), 2103-2116. DOI: 10.1056/NEJMoa1511939. View article
6. Uhlig, K., Patel, K., Ip, S., Kitsios, G. D., & Balk, E. M. (2013). Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Annals of internal medicine, 159(3), 185-194. View article
7. Fletcher, B. R., Hartmann-Boyce, J., Hinton, L., & McManus, R. J. (2015). The effect of self-monitoring of blood pressure on medication adherence and lifestyle factors: a systematic review and meta-analysis. American journal of hypertension, hpv008. View article
8. Ogedegbe, G., & Schoenthaler, A. (2006). A systematic review of the effects of home blood pressure monitoring on medication adherence. The Journal of Clinical Hypertension, 8(3), 174-180. View article
9. McManus, R. J., Mant, J., Roalfe, A., Oakes, R. A., Bryan, S., Pattison, H. M., & Hobbs, F. R. (2005). Targets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysis. Bmj, 331(7515), 493. View article
10. Margolis, K. L., Asche, S. E., Bergdall, A. R., Dehmer, S. P., Groen, S. E., Kadrmas, H. M., ... & O’Connor, P. J. (2013). Effect of Home Blood Pressure Telemonitoring and Pharmacist Management on Blood Pressure Control: A Cluster Randomized Clinical Trial. JAMA, 310(1), 46-56. DOI:10.1001/JAMA.2013.6549. View article
11. Neumann, C. L., Menne, J., Schettler, V., Hagenah, G. C., Brockes, C., Haller, H., & Schulz, E. G. (2015). Long-Term Effects of 3-Month Telemetric Blood Pressure Intervention in Patients with Inadequately Treated Arterial Hypertension. Telemedicine and E-Health, 21(3), 145-150. DOI: 10.1089/TMJ.2014.0058. View article
12. Zullig, L. L., Melnyk, S. D., Goldstein, K., Shaw, R. J., & Bosworth, H. B. (2013). The Role of Home Blood Pressure Telemonitoring in Managing Hypertensive Populations. Current Hypertension Reports, 15(4), 346-355. View article
13. Neumann, C. L., Menne, J., Rieken, E. M., Fischer, N., Weber, M. H., Haller, H., & Schulz, E. G. (2011). Blood Pressure Telemonitoring is Useful to Achieve Blood Pressure Control in Inadequately Treated Patients with Arterial Hypertension. Journal of Human Hypertension, 25(12), 732-738. View article
14. Fournier, J. C., DeRubeis, R. J., Hollon, S. D., Dimidjian, S., Amsterdam, J. D., Shelton, R. C., & Fawcett, J. (2010). Antidepressant Drug Effects and Depression Severity: A Patient-Level Meta-Analysis. JAMA, 303(1), 47-53. View article
15. Ogliari, G., Mahinrad, S., Stott, D. J., Jukema, J. W., Mooijaart, S. P., Macfarlane, P. W., ... & Sabayan, B. (2015). Resting Heart Rate, Heart Rate Variability and Functional Decline in Old Age. Canadian Medical Association Journal, 187(15), E442-E449. DOI:10.1503/CMAJ.150462. View article
16. Linden, W. (1984). Psychological Perspectives of Essential Hypertension: Etiology, Maintenance, and Treatment (Vol. 3). Karger Medical and Scientific Publishers.
17. Shapiro, A. P. (1996). Hypertension and Stress: A Unified Concept. Psychology Press.
18. Steptoe, A. (1986). Stress Mechanisms in Hypertension. Postgraduate Medical Journal, 62(729), 697-699. View article
19. Henry, J. P., Stephens, P. M., & Ely, D. L. (1986). Psychosocial Hypertension and the Defence and Defeat Reactions. Journal of Hypertension, 4(6), 687-688. View article
20. Markovitz, J. H., Matthews, K. A., Kannel, W. B., Cobb, J. L., & D'Agostino, R. B. (1993). Psychological Predictors of Hypertension in the Framingham Study: Is There Tension In Hypertension?. JAMA, 270(20), 2439-2443. View article
21. Gasperin, D., Netuveli, G., Dias-da-Costa, J. S., & Pattussi, M. P. (2009). Effect of Psychological Stress on Blood Pressure Increase: A Meta-Analysis of Cohort Studies. Cadernos de Saude Publica, 25(4), 715-726. View article
22. Tawakol, A., Ishai, A., Takx, R. A., Figueroa, A. L., Ali, A., Kaiser, Y., ... & Tang, C. Y. (2017). Relation Between Resting Amygdalar Activity And Cardiovascular Events: A Longitudinal And Cohort Study. The Lancet, 389(10071), 834-845. View article
23. American Heart Association (2014). High Stress, Hostility, Depression Linked with Increased Stroke Risk. View article
24. Lin, G., Xiang, Q., Fu, X., Wang, S., Wang, S., Chen, S., ... & Wang, T. (2012). Heart Rate Variability Biofeedback Decreases Blood Pressure in Prehypertensive Subjects by Improving Autonomic Function and Baroreflex. The Journal of Alternative and Complementary Medicine, 18(2), 143-152. View article
25. Gevirtz, R. (2013). The Promise of Heart Rate Variability Biofeedback: Evidence-Based Applications. Biofeedback, 41(3), 110-120. View article
26. Reinke, A., Gevirtz, R., & Mussgay, L, (2007). Effects of Heart Rate Variability Feedback in Reducing Blood Pressure [Abstract]. Applied Psychophysiology and Biofeedback, 32, 134.
27. Wang, S. Z., Li, S., Xu, X. Y., Lin, G. P., Shao, L., Zhao, Y., & Wang, T. H. (2010). Effect of Slow Abdominal Breathing Combined with Biofeedback on Blood Pressure and Heart Rate Variability in Prehypertension. The Journal of Alternative and Complementary Medicine, 16(10), 1039-1045. View article
28. Schein, M. H., Gavish, B., Herz, M., Rosner-Kahana, D., Naveh, P., Knishkowy, B., ... & Melmed, R. N. (2001). Treating Hypertension with a Device That Slows and Regularises Breathing: A Randomised, Double-Blind Controlled Study. Journal of Human Hypertension, 15(4), 271. View article
29. Yucha, C. B., Clark, L., Smith, M., Uris, P., LaFleur, B., & Duval, S. (2001). The Effect of Biofeedback in Hypertension. Applied Nursing Research, 14(1), 29-35. View article
30. Linden, W., & Moseley, J. V. (2006). The Efficacy of Behavioral Treatments for Hypertension. Applied Psychophysiology and Biofeedback, 31(1), 51-63. View article
31. Grossman, E., Grossman, A., Schein, M. H., Zimlichman, R., & Gavish, B. (2001). Breathing-Control Lowers Blood Pressure. Journal of Human Hypertension, 15(4), 263. View article
32. Rosenthal, T., Alter, A., Peleg, E., & Gavish, B. (2001). Device-Guided Breathing Exercises Reduce Blood Pressure: Ambulatory and Home Measurements. American Journal of Hypertension, 14(1), 74-76. View article
33. Meles, E., Giannattasio, C., Failla, M., Gentile, G., Capra, A., & Mancia, G. (2004). Nonpharmacologic Treatment of Hypertension by Respiratory Exercise in the Home Setting. American Journal of Hypertension, 17(4), 370-374. View article
34. del Paso, G. A. R., Cea, J. I., González-Pinto, A., Cabo, O. M., Caso, R., Brazal, J., ... & González, M. I. (2006). Short-Term Effects of a Brief Respiratory Training on Baroreceptor Cardiac Reflex Function in Normotensive and Mild Hypertensive Subjects. Applied Psychophysiology and Biofeedback, 31(1), 37-49. View article
35. Elliott, W. J., Izzo, J. L., White, W. B., Rosing, D. R., Snyder, C. S., Alter, A., ... & Black, H. R. (2004). Graded Blood Pressure Reduction in Hypertensive Outpatients Associated with Use of a Device to Assist with Slow Breathing. The Journal of Clinical Hypertension, 6(10), 553-559. View article
36. Bertisch, S. M., Schomer, A., Kelly, E. E., Baloa, L. A., Hueser, L. E., Pittman, S. D., & Malhotra, A. (2011). Device-Guided Paced Respiration as an Adjunctive Therapy for Hypertension in Obstructive Sleep Apnea: A Pilot Feasibility Study. Applied Psychophysiology and Biofeedback, 36(3), 173-179. View article
37. Nolan, R. P., Floras, J. S., Harvey, P. J., Kamath, M. V., Picton, P. E., Chessex, C., ... & Talbot, D. (2010). Behavioral Neurocardiac Training in Hypertension. Hypertension, 55(4), 1033-1039. DOI: 10.1161/HYPERTENSION-AHA.109.146233. View article
38. Viskoper, R., Shapira, I., Priluck, R., Mindlin, R., Chornia, L., Laszt, A., ... & Alter, A. (2003). Nonpharmacologic Treatment of Resistant Hypertensives by Device-Guided Slow Breathing Exercises. American Journal of Hypertension, 16(6), 484-487. View article
39. García-Vera, M. P., Labrador, F. J., & Sanz, J. (1997). Stress-Management Training for Essential Hypertension: A Controlled Study. Applied Psychophysiology and Biofeedback, 22(4), 261-283. DOI:10.1023/A:1022248029463. View article
40. Parati G, Izzo JL Jr, Gavish B., Third Edition. JL Izzo and HR Black, Eds. (2003). Respiration and Blood Pressure. Hypertension Primer (Ch. A40, p117-120). Baltimore, Lippincott Williams & Wilkins.
41. Hering, D., Kucharska, W., Kara, T., Somers, V. K., Parati, G., & Narkiewicz, K. (2013). Effects of Acute and Long-Term Slow Breathing Exercise on Muscle Sympathetic Nerve Activity in Untreated Male Patients with Hypertension. Journal of Hypertension, 31(4), 739-746. View article
42. Modesti, P. A., Ferrari, A., Bazzini, C., & Boddi, M. (2015). Time Sequence of Autonomic Changes Induced by Daily Slow-Breathing Sessions. Clinical Autonomic Research, 25(2), 95-104. DOI:10.1007/s10286-014-0255-9. View article
43. Joseph, C. N., Porta, C., Casucci, G., Casiraghi, N., Maffeis, M., Rossi, M., & Bernardi, L. (2005). Slow Breathing Improves Arterial Baroreflex Sensitivity and Decreases Blood Pressure in Essential Hypertension. Hypertension, 46(4), 714-718. View article
44. Elliott, W. J., & Izzo Jr, J. L. (2006). Device-Guided Breathing to Lower Blood Pressure: Case Report and Clinical Overview. Medscape General Medicine, 8(3), 23. View article
45. Wang, S. Z., Li, S., Xu, X. Y., Lin, G. P., Shao, L., Zhao, Y., & Wang, T. H. (2010). Effect of Slow Abdominal Breathing Combined with Biofeedback on Blood Pressure and Heart Rate Variability in Prehypertension. The Journal of Alternative and Complementary Medicine, 16(10), 1039-1045. DOI: 10.1089/acm.2009.0577. View article
46. Brook, R. D., Appel, L. J., Rubenfire, M., Ogedegbe, G., Bisognano, J. D., Elliott, W. J., ... & Rajagopalan, S. (2013). Beyond Medications and Diet: Alternative Approaches to Lowering Blood Pressure. Hypertension, 61(6), 1360-1383. DOI: 10.1161/HYP.0b013e318293645f. View article
47. Benson, H., Marzetta, B., Rosner, B., & Klemchuk, H. (1974). Decreased Blood-Pressure in Pharmacologically Treated Hypertensive Patients Who Regularly Elicited the Relaxation Response. The Lancet, 303(7852), 289-291. View article
48. Irvine, M. J., Johnston, D. W., Jenner, D. A., & Marie, G. V. (1986). Relaxation and Stress Management in the Treatment of Essential Hypertension. Journal of Psychosomatic Research, 30(4), 437-450. View article
49. Patel, C. (1975). 12-Month Follow-Up of Yoga and Bio-Feedback in the Management of Hypertension. The Lancet, 305(7898), 62-64. View article
50. Howorka, K., Pumprla, J., Tamm, J., Schabmann, A., Klomfar, S., Kostineak, E., ... & Sovova, E. (2013). Effects of Guided Breathing on Blood Pressure and Heart Rate Variability in Hypertensive Diabetic Patients. Autonomic Neuroscience, 179(1), 131-137. View article
51. Schneider, R. H., Alexander, C. N., Staggers, F., Rainforth, M., Salerno, J. W., Hartz, A., ... & Nidich, S. I. (2005). Long-Term Effects of Stress Reduction on Mortality in Persons≥ 55 Years of Age with Systemic Hypertension. The American Journal of Cardiology, 95(9), 1060-1064. View article
52. Brook, R. D., Appel, L. J., Rubenfire, M., Ogedegbe, G., Bisognano, J. D., Elliott, W. J., ... & Rajagopalan, S. (2013). Beyond Medications and Diet: Alternative Approaches to Lowering Blood Pressure. Hypertension, 61(6), 1360-1383. DOI: 10.1161/HYP.0b013e318293645f. View article
53. Lehrer, P. M., & Gevirtz, R. (2014). Heart Rate Variability Biofeedback: How and Why Does it Work?. Frontiers in Psychology, 5, 756. View article
54. Fournier, J. C., DeRubeis, R. J., Hollon, S. D., Dimidjian, S., Amsterdam, J. D., Shelton, R. C., & Fawcett, J. (2010). Antidepressant Drug Effects and Depression Severity: A Patient-Level Meta-Analysis. JAMA, 303(1), 47-53. View article
55. Kirsch, I., Deacon, B. J., Huedo-Medina, T. B., Scoboria, A., Moore, T. J., & Johnson, B. T. (2008). Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration. PLoS Med, 5(2), e45. View article
56. Turner, E. H., Matthews, A. M., Linardatos, E., Tell, R. A., & Rosenthal, R. (2008). Selective Publication of Antidepressant Trials and Its Influence on Apparent Efficacy. New England Journal of Medicine, 358(3), 252-260. View article